Medical Professionals
The Development of a New Orbital Implant
The Bio-eye orbital hydroxyapatite (HA) implant was conceived by Arthur C. Perry, M.D., in the early 1980s, after a comprehensive review of the literature on orbital implants, which included the earliest manuscripts dating back to 1885 (Mules 1885). This review, along with an ongoing dissatisfaction with the performance of contemporary implants, allowed Perry to identify the performance characteristics of an ideal orbital implant and, perhaps more importantly, led to the identification of the key physical design variables that accounted for the relative success or failure of a given orbital implant
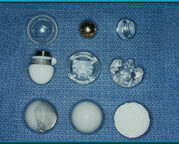
Figure 1: Orbital Implants of Various Designs and Materials
implant in the upper left is a hollow glass ball, as first used by Mules in 1884. Also shown are implants of gold, silicone, and acrylic in various shapes. Middle left: a Troutman implant containing a magnet to hold the artificial eye. Bottom right: the Bio-eye hydroxyapatite orbital implant.
While the Bio-eye orbital implant is a major improvement over traditional implants (see figure 1), the goal of creating an ideal orbital implant has yet to be reached, since, as an ideal invention, it must do much more than simply mimic the natural eye: it must improve upon the natural eye’s visual acuity, the field of view, disease resistance, psycho-social responsiveness, information-carrying rate and capacity, upgradeability, etc.
The first step in the quest for an ideal implant, however, began with a focus on the less-glamorous but more manageable problem of reducing the complications common to existing synthetic implants. The basic strategy was to develop an orbital implant that incorporated all of the design features that the literature review had shown to be common features of the most successful implant designs. These features, and their constraints, can be summarized as follows:
-
Maintain Natural Lid Shape
The implant must provide a means, such as the ability to receive a motility/support peg, to support the weight of the artificial eye to prevent damage to the delicate muscles of the lower lids over time.
-
Light Weight
The implant must be light in weight.
-
Porosity
The implant must allow vascular orbital tissues to invade its structure to: a) lock it into place and prevent migration, b) allow it to fight infections from within the implant via the vascular bed infiltrating the implant, and c) support “healing from within” of any defect in the conjunctival-Tenon’s closure.
-
True Integration
The implant must be directly integrated (e.g., via a peg) with the artificial eye to allow direct transfer of all available movement from the rectus muscles to the artificial eye.
-
Natural Biocompatibility
The implant must be a natural material and readily accepted by the tissues of the orbit to prevent “synthetic implant syndrome” i.e., pseudocapsule formation around the implant. This pseudocapsule is the body’s way of walling off a foreign material.
The Bio-eye orbital implant was specifically designed to incorporate each of these features. However, the story of its development is one of serendipitous discovery as much as it is of medical invention. Some years earlier, it had been discovered that certain species of marine coral have a skeleton with a microarchitecture almost identical to that of human cancellous bone.
Fortunately, these species also have a chemical makeup that allows them to be converted to hydroxyapatite (HA), which is the mineral that makes up the hard portion of bone. This remarkable coincidence enables converted coral implants to be invisible to the immune system, preventing the implant from producing a foreign body reaction that has been a complication of implants for over 100 years. Both X-ray diffraction and SEM microscopy have shown naturally derived HA to be virtually identical to the mineral portion of cancellous bone in terms of both porosity and chemical makeup. Consequently, soft tissue readily infiltrates the material, muscles can be attached to it, and, if exposed, the material tends to “heal” itself using the body’s natural mechanisms for wound closure and infection resistance.
Reports indicate that the natural Bio-eye orbital implant significantly reduces the incidence of complications associated with traditional synthetic orbital implants, such as those composed of silicone or plastic (polymethyl methacrylate) and has the ability to greatly increase artificial eye movement. (Hornblass 1992, Perry 1990). Historically, the use of nonporous synthetic orbital implants has led to complications such as exposure, extrusion, migration, infection, poor motility, and poor cosmesis.
The natural Bio-eye orbital implant achieved its success because it is highly biocompatible and completely porous. Hydroxyapatite is a complex calcium phosphate, which is the same mineral that comprises the hard portion (mineral portion) of human bone, and is therefore readily accepted by the tissues of the orbit. Additionally, natural hydroxyapatite is derived from a specific genus of marine coral whose exoskeleton is completely porous: each pore connects with every other pore. This is an extremely important characteristic for long-term success. Synthetic orbital implants silicon, polyethylene, porous polyethylene (like Medpor) and aluminum oxide (like Bioceramics) have been unable to duplicate the complete interconnective characteristic of natural hydroxyapatite. Natural HA also matches the 500µ pore size characteristic of human cancellous bone (Piecuch 1982), which, by volume, is 50% hard tissue and 50% soft tissue. When placed into the orbit, natural HA becomes fully incorporated with the fibrovascular tissues of the orbit, and when attached to the rectus muscles, can deliver all available socket motility directly to the artificial eye.
Additionally, the natural hydroxyapatite orbital implant has the longest successful track record of any known implant material that can successfully accommodate a motility/support peg, which directly connects the artificial eye to the implant. The complete interconnected porosity filled with fibrovascular ingrowth makes this possible. The motility/support peg supports the weight of the prosthesis while simultaneously ensuring transfer of any socket movement directly to the prosthesis.

